IBS. Three little letters that carry a lot of weight. More commonly known as Irritable Bowel Syndrome, it’s a common chronic functional gastrointestinal disorder that causes pain, discomfort, bloating, and altered bowel habits.
The global presence is 11.2% but the incidence of the disease is higher in western countries affecting 10-20% of the adult population and twice as likely among women.
The mechanism remains unclear but altered gastrointestinal motility, changes to gut microbiota, altered brain gut axis, low grade digestive track inflammation and psychological factors may all play a role.
There is currently no diagnostic biomarker for IBS so it is often diagnosed based of symptoms using what’s called the Rome IV criteria and ruling out celiac disease. Rome IV criteria require the presence of recurrent abdominal pain, associated with two or more of
- pain related to defecation
- change in frequency and/or form of stool
- additional symptoms such as abdominal pain, bloating, acid regurgitation, nausea, vomiting, distention, and borborygmus aka belching.
That is a lot of discomfort for nearly 20% of adults to experience on a regular basis. Or perhaps, irregular basis is more accurate.
With so many potential factors contributing to IBS, dietary triggers are reported to be central to the symptom affecting 50-84% of patients with IBS.
The most commonly reported foods that trigger these symptoms are those containing lactose (e.g. milk); fructose (e.g. honey, dates, oranges, cherries, apples, and pears); gas producing foods (e.g. beans cabbage and bran); and sweeteners (e.g. sorbitol, mannitol and xylitol). This would suggest that dietary interventions excluding these common triggers may be helpful treatment.
But what is the common thread among these foods?
Three little letters have met their six-letter match. FODMAP. No, its not a video game, or a shake supplement or trending internet meme. Its an acronym used to describe
Fermentable
Oligosaccharide
Disaccharide
Monosaccharide
And
Polyols.
But wait. You’re not a scientist and have never heard of these things before. How on earth is this supposed to help you avoid chronic stomach pain and trips to the bathroom?
Simply put, these complicated sounding terms are the highly fermentable components of carbohydrates that cause an increase of gas, bloating, and stomach discomfort. Ever have a beer? Or if you’re under 21, Kombucha? Then you may know it is fermented, giving it that bubbly taste. Fermentation is the enzymatic or bacterial extraction of energy from carbohydrates in the absence of oxygen, producing carbon dioxide as a result. Well that’s exactly what these carbohydrate components do in your stomach. And when they ferment in your gut, they increase the water content into your bowel and increase gas by feeding your colonic bacteria. Sort of like yeast feeding on sugars to make your beer both alcoholic and fizzy.
Now that you understand the concept, lets dive into a little more of where to find these culprits.
Oligosaccharides are made of small bunches of monosaccharides aka the tiny little building blocks of all carbohydrates. They include fructans (e.g. wheat, onion and garlic) as well as alpha galacto-oligosaccharides (e.g. beans and pulses). All humans lack enzymes that hydrolyze these therefore they aren’t able to be digested and absorbed. Instead they get fermented by the colon, causing gas and in those with IBS, additional symptoms.
Lactose in milk is an example of a disaccharide, or 2 monosaccharides bonded together, which requires the enzyme lactase in order to be digested. Without that enzyme, water is drawn into the colon to dilute the lactose and it’s fermented by your gut bacteria creating gas and distension.
Fructose is a monosaccharide that some people aren’t able to absorb. Glucose is another monosaccharide but helps with fructose metabolism. If fructose is present in high concentrations like in, say, fruit juice or soda, it can lead to high levels of fructose in the small intestine which increases small intestinal water and may lead to an array of gut symptoms like diarrhea. This is actually how prune juice and apple juice help when little kids are constipated.
Polyols include sorbitol (e.g. apple and pear), mannitol (e.g. mushroom and cauliflower) and xylitol (e.g. artificial sweeteners) and are passively absorbed along the small intestine. For those sensitive to foods high in Polyols there may be an increase of small intestinal water and as a result, gut discomfort.
The aim of a low FODMAP diet is to eliminate higher FODMAP items for a period of up to 4 weeks and slowly begin reintroducing them one at a time in a period of 3-day intervals of increasing amounts. For example, adding mango for 3 days to establish tolerance for fructose or bread, onions or garlic to establish tolerance for fructans.
Several meta-analysis and cohort studies have shown that between 57-72.1% of patients experience relief when participating in modified FODMAP diet planning. One study concludes, “a low FODMAP diet significantly improves general symptoms in patients with IBS compared to standard dietary recommendations with high FODMAP foods”.
Great. There is a credible solution to your chronic stomach pain: avoid high FODMAP foods but….. what are they?!! Great question. If you can’t remember how many calories were in your cereal, how could you possibly know how much fructan is in….wait what is a fructan again?
Fortunately, a group of scientists did the work to provide the answers for you.
Lactose was first studied in the 1950s, Fructose and polyols in the 1970s and eventually fructans by 1987. But a group of scientists from Monash University in Australia (named the Monash group) decided to group these culprits together using the term FODMAP in 2004 and published their research hypothesis in Alimentary Pharmacology and Therapeutics in 2005. After their hypothesis was published, an intensive program of research was launched including a comprehensive analysis to determine the amount of FODMAPs in carbohydrate containing foods to come up with a comprehensive list and rating for nearly all foods to help the public navigate exactly what to eat. That list is now publicized on both www.ibsdiets.org as well as www.monashfodmap.com
But to help you get started, here’s a brief list 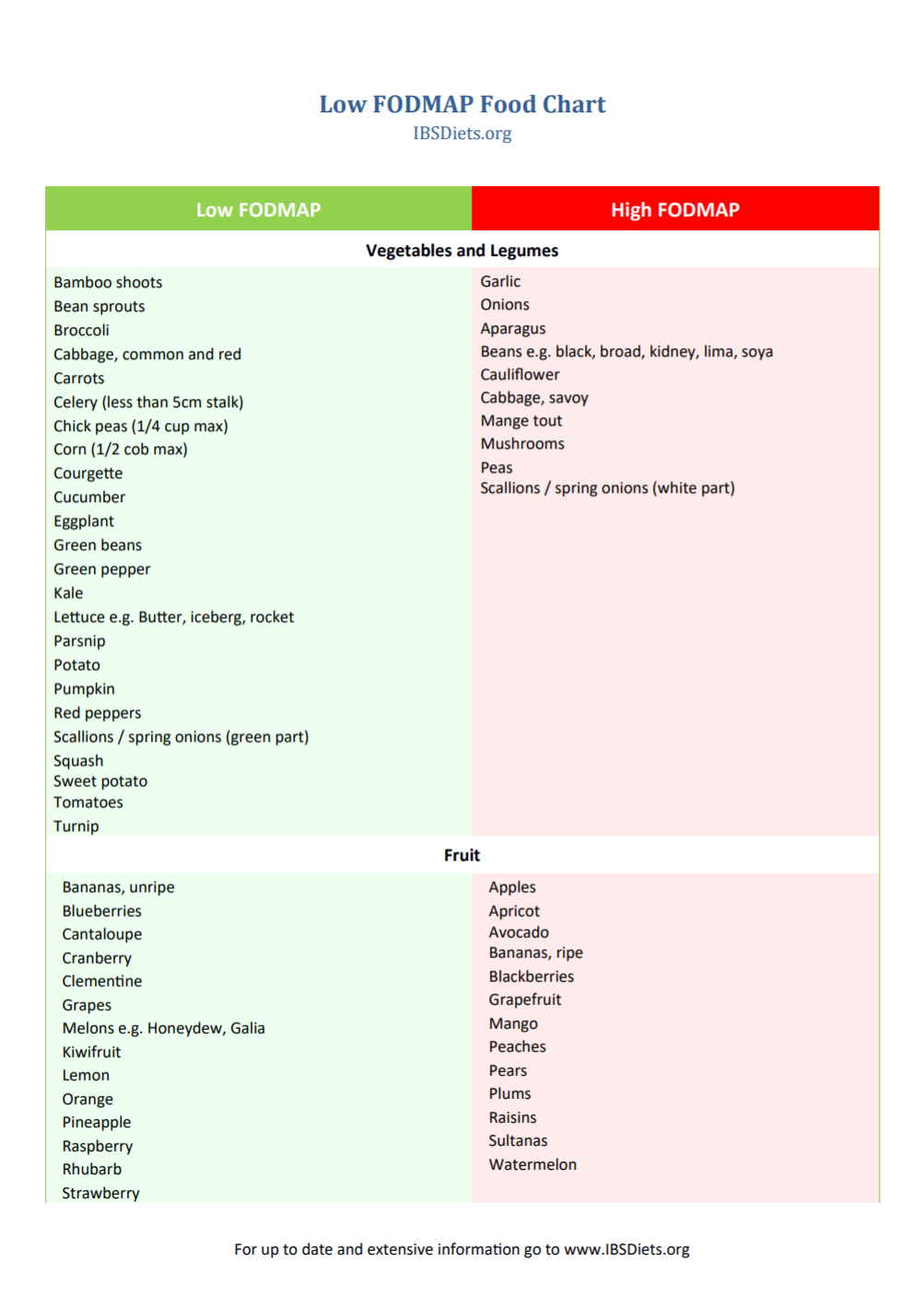
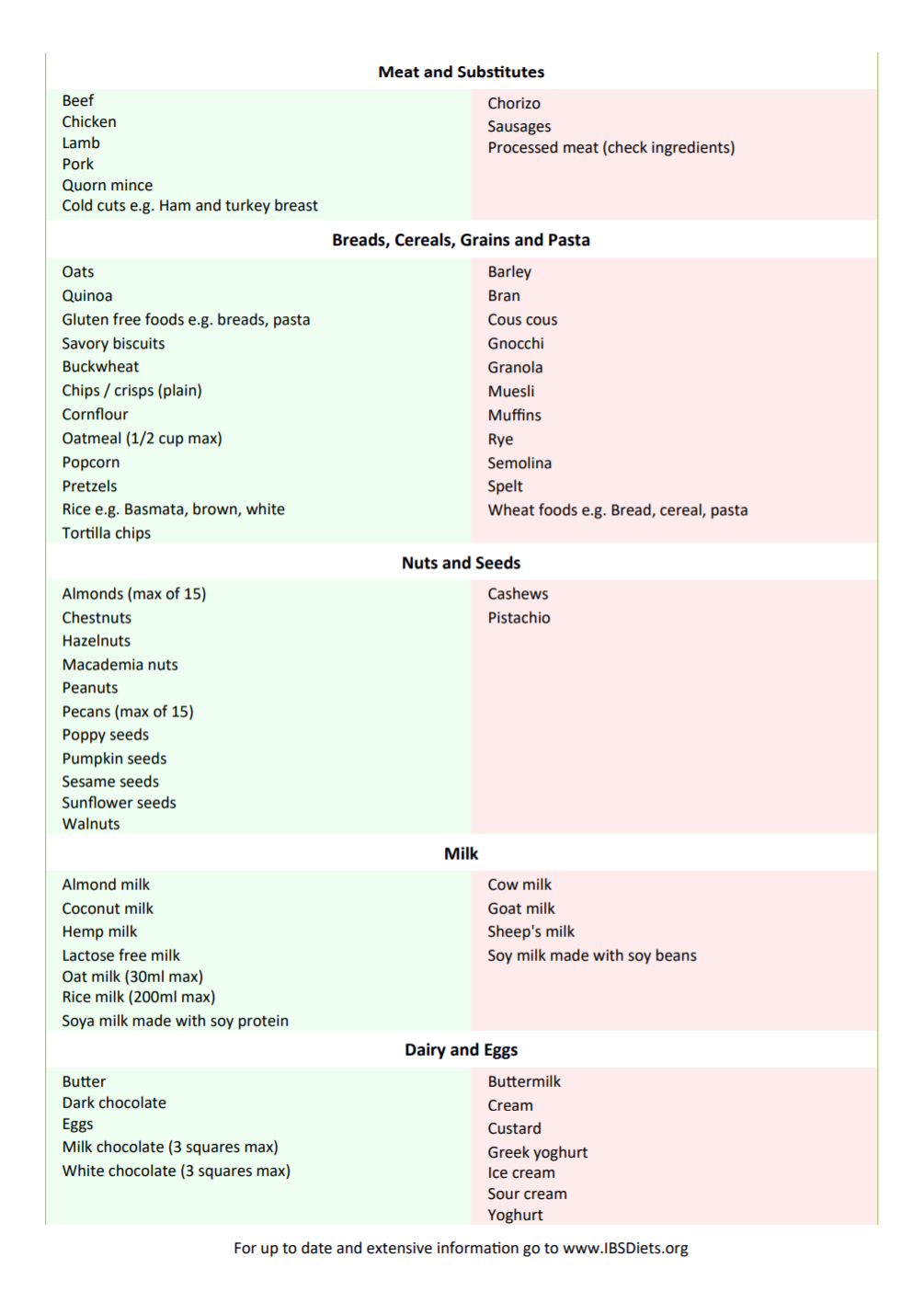
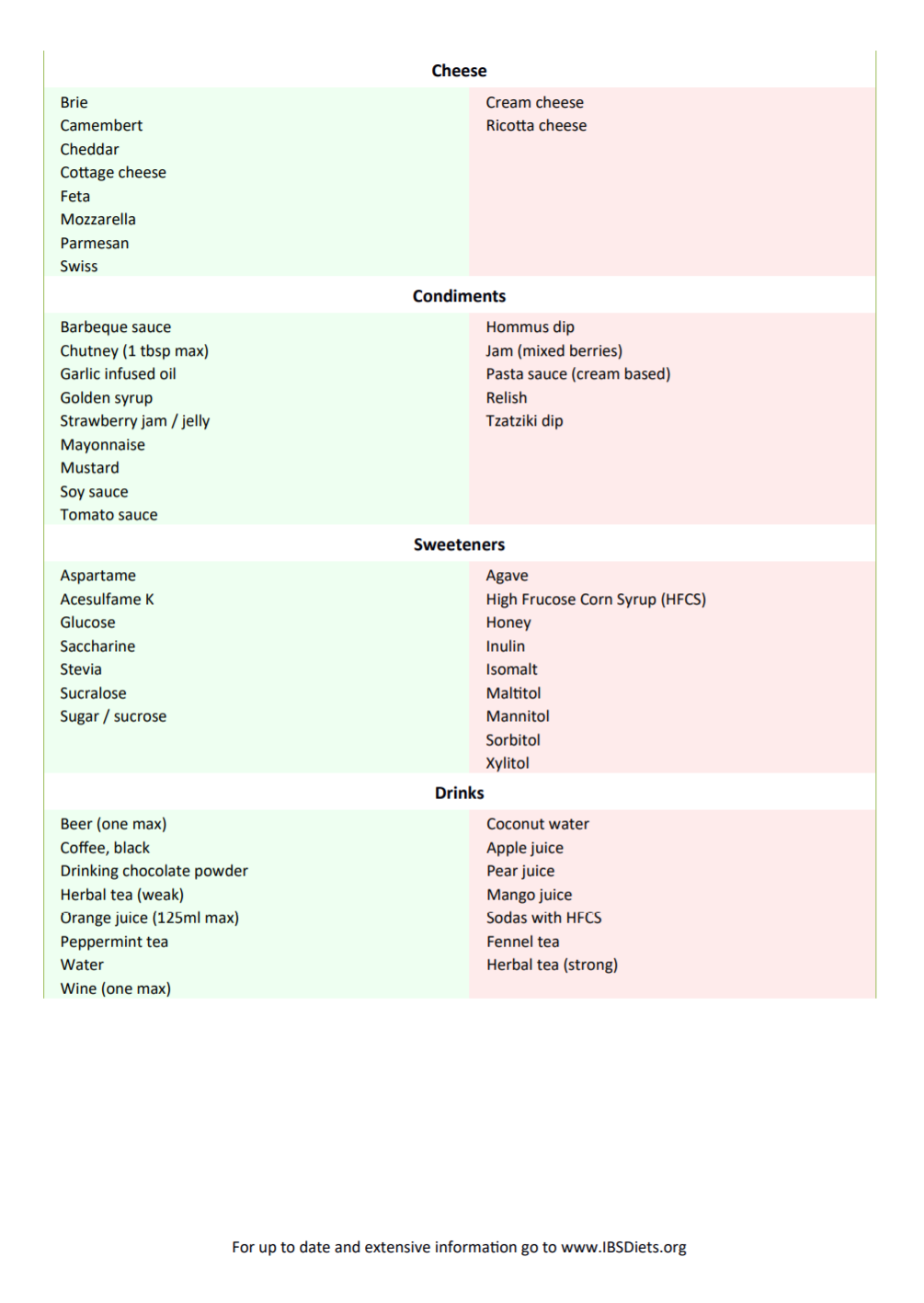
Having IBS doesn’t mean you have to abstain from all high FODMAP foods. Its completely possible that Asparagus has never bothered your stomach and never will. But with a map of possibilities, playing detective with your diet may lead you to discover after a few heavy garlic pastas followed by late nights full of Tums and Alka-Seltzer, garlic may be a trigger for you. The best way to navigate this labyrinth of food choices is by listening to your gut, literally. Pay attention to symptoms, keep a list handy of possible culprits, and work with a dietician on a plan to get you feeling better.
References
- Whelan K, Martin LD, Staudacher HM, Lomer MCE. The low FODMAP diet in the management of irritable bowel syndrome: an evidence-based review of FODMAP restriction, reintroduction and personalisation in clinical practice. Journal of Human Nutrition and Dietetics. 2018;31(2):239-255.
- Weynants A, Goossens L, Genetello M, Looze DD, Winckel MV. The long‐term effect and adherence of a low fermentable oligosaccharides disaccharides monosaccharides and polyols (FODMAP) diet in patients with irritable bowel syndrome. Journal of Human Nutrition and Dietetics. 2019;33(2):159-169.
- Gibson PR. History of the low FODMAP diet. Journal of Gastroenterology and Hepatology. 2017;32:5-7 https://onlinelibrary.wiley.com/doi/pdf/10.1111/jgh.13685