Meal planning with Diabetes can be done by following some simple guidelines. The most important thing to think about when you are living with diabetes is to chose a diet that is balanced in carbohydrates, protein and fat to help stabilized blood sugar. Carbohydrates are what raises blood sugar, and some raise blood glucose more than others. Refined carbohydrates, where the fiber has been eliminated or reduced, have a greater impact on raising blood glucose levels. These include foods such as white breads, pastas, and crackers, cookies, candy, and softdrinks or juice. Choosing carbohydrates that are high in fiber, such as whole grains, leafy green and cruciferous vegetables, nuts, seeds, and berries can help keep your blood sugar more stable. Lean protein sources like beans, tofu, and lean meats are great to include at every meal. Healthy fat sources include nuts, seeds, avocados, and olive oil. The American Diabetes Association recommends the nutrients Vitamin D, Calcium, Omega 3 fats and Fiber to stabilize blood sugar, and increase insulin sensitivity. Dairy products like skim milk or yogurt are great sources of Calcium while whole grains fruits and vegetables contain fiber. Omega-3 fats are found in many fish, nuts, seeds, and liquid oils. Build your daily meal plan by choosing one breakfast, one lunch and one dinner, plus two snacks.
Glycemic Index and Diabetes
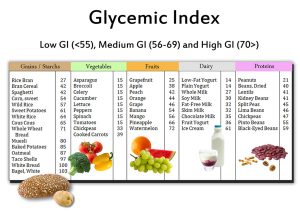
The glycemic index, or GI, measures how a carbohydrate-containing food raises blood glucose. Foods are ranked based on how they compare to a reference food — either glucose or white bread.
A food with a high GI raises blood glucose more than a food with a medium or low GI.
Meal planning with the GI involves choosing foods that have a low or medium GI. If eating a food with a high GI, you can combine it with low GI foods to help balance the meal.
Examples of carbohydrate-containing foods with a low GI include dried beans and legumes (like kidney beans and lentils), all non-starchy vegetables, some starchy vegetables like sweet potatoes, most fruit, and many whole grain breads and cereals (like barley, whole wheat bread, rye bread, and all-bran cereal).
Meats and fats don’t have a GI because they do not contain carbohydrate.
Using the carbohydrate exchange counting system, here is a Type II Diabetes friendly sample 1 day menu.
| Food | Amount | Servings Provided |
| Breakfast | ||
| Egg white omelet with: | 3 egg whites, 1 yolk | 3 protein, 1 omega-3 |
| Green peppers,
Onions | ½ Cup Peppers, ¼ Cup Onion | 1 vegetable |
| Low fat cheese | ½ Cup Cheese | 1 dairy |
| Orange Juice | 8oz | 1 fruit |
| 1 slice wheat toast with “olivo” spread | 1 slice | 1 grain, 1 omega-3 |
| Lunch | ||
| Salad with tomato and: | 2 cups spring mix, ½ tomato | 2 servings veggie |
| Tuna | 3oz | 1 protein, 1 omega-3 |
| Olive oil + lemon dressing | 2 TBS | 1 omega-3 |
| Banana | 1 banana | 1 fruit |
| Whole Wheat Crackers | 16 crackers | 1 grain |
| Dinner | ||
| 3 oz Chicken Breast | 3 oz | 1 protein |
| Brown Rice w/ “olivo” spread | ½ Cup | 1 grain |
| Steamed Vegetable Medley (broccoli, cauliflower, carrots) | ½ Cup | 2 veggie / 1 fiber |
| Whole Wheat Roll | 1 oz | 2 grains |
| Snacks | ||
| 1 Glass of milk w/ skim or soy milk | 1Cup Milk, | 1 serving Milk, 30% DV calcium |
| Apple with organic almond butter | 1 apple, 2tbs PB | 1 fruit, 1 mono-unsaturated fat |
| Raw vegetables (broccoli, carrots, peppers) w/ low fat ranch or hummus | 1 cup per snack, up to 2x daily | 4 veggie, 2 fiber |
| Fat free yogurt w/ berries and granola | 6oz yogurt, ½ cup berries, ¼ Cup granola | 1 dairy, 1 protein, 1 fruit, ½ grain |